Dec 7
2016
Four Steps to Value-Based Care Success in 2017 Under the MACRA Final Rule
Guest post by Richard Loomis, MD, chief medical officer and VP of informatics, Practice Fusion.

If you bill Medicare, changes are coming in 2017 that may affect your reimbursements. Existing programs such as the electronic health record (EHR) Incentive Program (meaningful use) and the Physician Quality Reporting System (PQRS) are being replaced by a new payment system called the Quality Payment Program (QPP), which is a complex, multi-track program that will adjust payments from -9 percent to +37 percent by 2022. The Centers for Medicare & Medicaid Services (CMS) recently released the final rule that will implement the QPP as part of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).
While the 2,300-page final rule outlining the new program is complex, successful participation in 2017 doesn’t have to be. Here are some tips on how to participate in the QPP starting January 1, 2017 to minimize the risk of any negative adjustment to your Medicare Part B payments beginning in 2019.
Step 1: Check if you qualify to participate
CMS has expanded the range of clinicians able to participate in the QPP compared to Meaningful Use (MU). Eligible clinicians now include physicians, physician assistants, nurse practitioners, clinical nurse specialists and certified registered nurse anesthetists. However, you’re excluded from participating in 2017 if:
- You’re a clinician enrolling in Medicare for the first time. You’re exempt from reporting on measures and activities for the Merit-Based Incentive Payment System (MIPS) until the 2018 performance year.
- Your practice meets the low-volume threshold. This means your Medicare Part B allowed charges ? $30,000 OR you see ? 100 patients covered by Medicare Part B during the 2017 calendar year.
Step 2: Choose your participation track
Although the QPP will begin January 1, 2017, there will be a ramp-up period with less financial risk for eligible clinicians in at least the first two years of the program. CMS designated 2017 as a transition year to help providers get started in either of the two participation tracks: MIPS or the Advanced Alternative Payment Models (Advanced APMs).
MIPS
MIPS streamlines current Medicare value and quality program measures — PQRS, Value Modifier (VM) Program and MU — into a single MIPS composite performance score that will be used to adjust payments. All eligible clinicians who are not participating in an Advanced APM should report under MIPS in 2017. Conversely, you’re not required to participate in MIPS if you’re participating in an eligible Advanced APM, as described below. Some APMs, by virtue of their structure, are not considered Advanced APMs by CMS. If you participate in an APM that doesn’t qualify as an Advanced APM, it will increase your favorable scoring under the MIPS participation track.
Advanced APMs
APMs are new approaches to paying for medical care through Medicare that provide incentive payments to support high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population. The main difference between the MIPS and Advanced APM programs are that Advanced APMs require practices to take on more financial and technological risks.
Advanced APMs meet specific criteria from CMS. Those who participate in Advanced APMs, including the Comprehensive Primary Care Plus (CPC+), may be determined to be qualifying APM participants (QPs), and receive the following benefits:
- QPs are not subject to MIPS.
- They receive a five percent lump sum bonus payments for the years 2019-2024.
- They will receive a higher fee schedule update for 2026 and onward.
It’s important to note that if you stop participating in an Advanced APM during 2017, you should make sure you’ve seen enough patients or received enough payments through an Advanced APM to qualify for the five percent bonus. If you haven’t met these thresholds, you may need to participate in MIPS reporting to avoid a negative payment adjustment.
Step 3: Choose your pace of participation
CMS designated 2017 as a transition year that allows eligible clinicians to pick their pace of participation for the program’s first performance period beginning Jan. 1, 2017. By creating a flexible reporting structure, CMS hopes to encourage clinician participation from the start by providing a period of interactive learning and development.
If you’re participating under the MIPS track in 2017, you can test the program, report a partial year, or submit data for the full year:
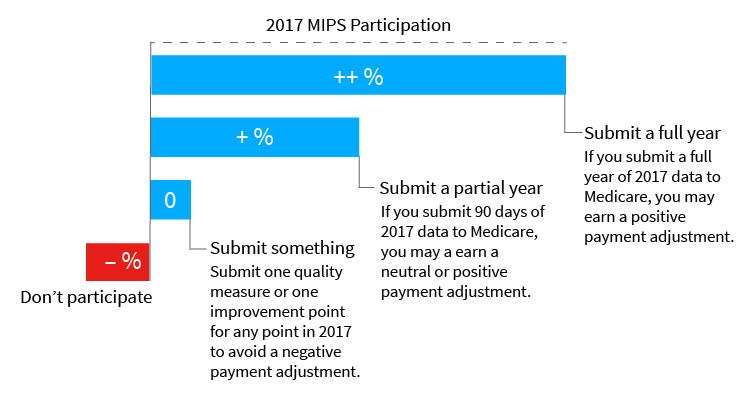
The size of your payment will depend both on how much data you submit and your performance results. Since the QPP is cost neutral, the size of your positive adjustment also depends on how many eligible clinicians do not participate in the program and receive a negative adjustment. If you don’t submit any 2017 data, then you receive a negative four percent payment adjustment on your Medicare Part B payments in 2019.
Step 4: Use a certified EHR to meet quality measures and reporting
Both participation tracks require the use of certified EHR technology to meet measures, including patient engagement and care coordination. Confirm with your EHR vendor if your EHR is currently certified to help you participate in the QPP, and if they plan to maintain certification by meeting the latest Office of the National Coordinator for Health Information Technology (ONC) requirements that vendors must implement by 2018.
Ultimately, CMS is estimating 90 percent of eligible clinicians will receive a positive or neutral MIPS adjustment for the 2017 transition year, but it’s our hope every eligible clinician will avoid a negative payment adjustment by successfully participating in the Quality Payment Program.
If Obamacare is abolished, will this be abolished with it?