Apr 23
2019
eConsult Platform Use In Community Primary Care Settings Reduces Uncompensated Care Provided By Hospitals
By Chris Jaeger, head of ACO and health system strategy, AristaMD.
Rural hospitals are facing severe challenges in maintaining operating margin, with uncompensated care being a major factor. Telehealth eConsult platform use in local primary care settings to improve “right time, right place, right provider care” have been shown to decrease the number of patients receiving avoidable and unnecessary care within the hospital setting, thus supporting hospital’s ability to mitigate uncompensated care.
Uncompensated care is an overall measure of hospital care provided for which payment was not received from the patient or payer group. It equates to the sum of a hospital’s bad debt — the financial assistance it provides. Financial assistance includes care for which hospitals never expected to be reimbursed and care provided at a reduced cost for those in need. A hospital incurs bad debt when it cannot obtain re-imbursement for care provided; this happens when patients are unable to pay their bills, but do not apply for financial assistance, or are unwilling to pay their bills.
Hospitals, both nonprofit and for-profit, provide uncompensated care for individuals who are uninsured and under insured.
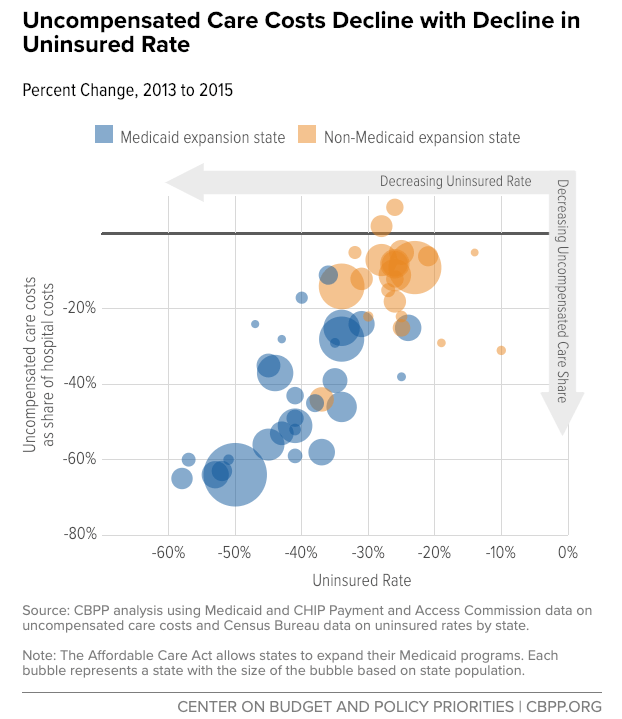
Though there has been a noted decline in uncompensated care since the 2014 passage of the Affordable Care Act and Medicaid expansion, this has not carried over to states not part of the expansion. States that expanded Medicaid to low-income adults under the ACA recognized a 47 percent decrease in uncompensated care costs, on average, compared to an 11 percent decrease in states that did not expand Medicaid.
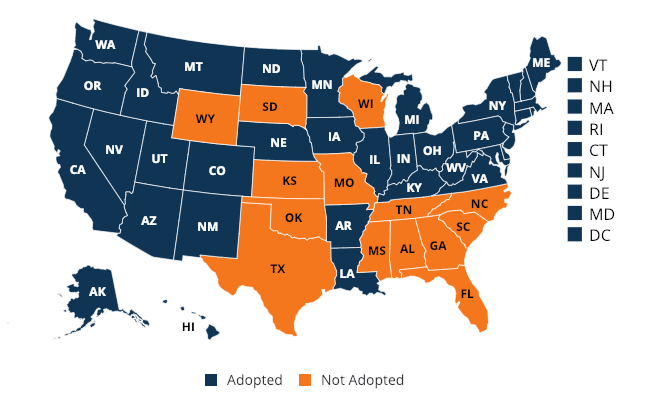
(Coverage map as of Feb 2019)
Uncompensated care and dropping revenue margins are causing hospitals, especially in rural areas, to close. “While Medicaid expansion has improved all hospitals’ operating margins and total margins, the effect was particularly pronounced in rural areas,” noted a report from the Center on Budget and Policy Priorities. A recent study by the North Carolina Rural Health Research Program (NC-RHRP) at the University of North Carolina Cecil G. Sheps Center for Health Services Research (UNC-CH) showed that since 2010, 89 rural hospitals in 26 states have closed.
Much of this uncompensated care could be prevented through primary care intervention. A report, released by Premier, found that six common chronic conditions accounted for 60 percent of 24 million Emergency Department (ED) visits in 2017; out of that 60 percent, approximately one third of the visits (4.3 million) were likely preventable and could be treated in a less expensive outpatient setting.