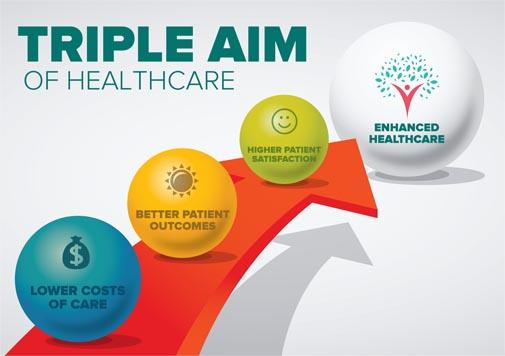
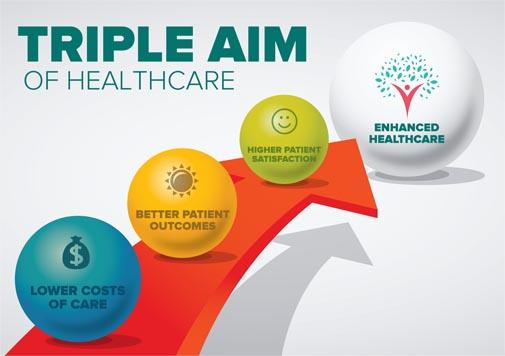
 The Triple Aim framework has emerged as a guiding principle for healthcare organizations seeking to optimize patient care outcomes while simultaneously containing costs.
The Triple Aim framework has emerged as a guiding principle for healthcare organizations seeking to optimize patient care outcomes while simultaneously containing costs.
Developed by the Institute for Healthcare Improvement (IHI), the Triple Aim provides a holistic approach to healthcare delivery by focusing on three interrelated goals: improving population health, enhancing patient experience, and reducing healthcare costs.
This article aims to delve into the rationale behind the Triple Aim, its intended objectives, and its profound impact on health systems and medical providers.
The Need for a Transformation
The United States, like many other nations, faces several healthcare challenges, including escalating costs, inconsistent quality of care, and fragmented systems. The existing fee-for-service model has contributed to excessive healthcare spending without necessarily translating into improved patient outcomes. Consequently, the need for a fundamental transformation in healthcare delivery arose, giving rise to the Triple Aim.
The Triple Aim Explained: Improve Population Health
The first aim of the Triple Aim is to improve the overall health of populations. This involves addressing the determinants of health, promoting preventive care, and implementing evidence-based interventions to manage chronic diseases effectively. By focusing on population health, healthcare providers aim to reduce the incidence of preventable diseases and enhance the overall well-being of communities.
Enhance Patient Experience
The second aim of the Triple Aim is to enhance the patient experience of care. This encompasses various aspects, including improving access to care, fostering effective communication between patients and providers, ensuring care coordination, and respecting patients’ preferences and values. Patient-centered care lies at the heart of this aim, striving to create a healthcare system that meets the unique needs and expectations of each individual.
Reduce Healthcare Costs
The third aim of the Triple Aim seeks to reduce healthcare costs without compromising the quality of care. Healthcare systems are encouraged to adopt innovative approaches to resource management, eliminate waste, and streamline processes to achieve financial sustainability. By addressing inefficiencies and focusing on cost-effective care, the Triple Aim aims to make healthcare more affordable and accessible for all.
Continue Reading
 In the previous articles, we discussed the importance of healthcare interoperability and the factors hindering its progress. In this final part, we will explore potential solutions and future directions to accelerate the advancement of interoperability in healthcare.
In the previous articles, we discussed the importance of healthcare interoperability and the factors hindering its progress. In this final part, we will explore potential solutions and future directions to accelerate the advancement of interoperability in healthcare.
Standardization and Data Exchange Frameworks
One of the key solutions for promoting interoperability is the adoption of standardized data formats and exchange frameworks. Implementing widely accepted standards, such as HL7 FHIR (Fast Healthcare Interoperability Resources), can facilitate seamless data exchange between different systems. Embracing common standards ensures that healthcare organizations can effectively communicate and share information, regardless of the systems they use.
Enhancing Data Governance and Consent Management
To address privacy concerns and build trust, robust data governance frameworks and consent management mechanisms need to be established. Patients should have control over their health data, allowing them to provide informed consent for data sharing and specify their privacy preferences. Implementing strong security measures, ensuring data integrity, and promoting transparent data handling practices are vital for fostering patient confidence in interoperability initiatives.
Continue Reading

In our previous article, we discussed the importance of healthcare interoperability and some of the challenges that impede its progress. In this second part, we will delve deeper into the factors that hinder the advancement of healthcare interoperability.
By understanding these barriers, we can work towards overcoming them and achieving a more interconnected healthcare system.
Fragmented Health IT Landscape
The healthcare industry operates within a fragmented landscape, with various electronic health record (EHR) systems, medical devices, and health information exchange (HIE) platforms in use. These systems often lack standardized data formats and interoperability capabilities, making it challenging to exchange information seamlessly.
The lack of a unified approach leads to data silos, where patient information becomes trapped within specific systems and organizations.
Proprietary Systems and Vendor Lock-In
Proprietary EHR systems and vendor lock-in practices can hinder interoperability. When healthcare organizations heavily invest in a particular vendor’s system, it may restrict their ability to share data with other systems or switch vendors.
This limited interoperability can impede the seamless exchange of patient information and hinder collaboration between healthcare providers.
Information Blocking Practices
Information blocking refers to practices that intentionally impede the access, exchange, or use of electronic health information. Although regulations such as the 21st Century Cures Act in the United States discourage information blocking, instances of such practices have been reported. Some vendors or healthcare organizations may restrict data sharing for competitive or financial reasons, hindering the free flow of information necessary for interoperability.
Continue Reading

Welcome to this three-part series examining healthcare interoperability in the United States and the reasons for its slow progress. In Part 1, we delve into the fragmented healthcare landscape and the technical challenges that impede seamless data exchange.
The Fragmented Healthcare Landscape
The need for interoperability in healthcare can be attributed to the fragmented landscape of the industry. In the United States, the healthcare ecosystem comprises a wide range of organizations, including hospitals, clinics, and specialty practices. Each operates with different electronic health record (EHR) systems, infrastructure, and data models, creating significant interoperability gaps.
The fragmented landscape hinders the seamless exchange of patient data and poses a barrier to efficient care delivery.
Technical Challenges
Technical challenges play a crucial role in impeding healthcare interoperability. One of the major obstacles is the diversity of data formats and standards used by different healthcare systems and EHR vendors. Historically, proprietary data formats were implemented by vendors, resulting in compatibility issues and difficulties in exchanging information between systems.
We have made strides in improving interoperability but are not where we need to be. It’s a complex issue that requires collaborative efforts among stakeholders to overcome technical and policy challenges. These technical challenges include data standardization, data exchange protocols, and semantic interoperability.
Legacy systems also contribute to the lack of interoperability. Many healthcare organizations still rely on outdated systems not designed with interoperability in mind. These legacy systems may need more capabilities or face compatibility issues with newer technologies, making sharing and exchanging patient data challenging.
The impact of legacy systems on interoperability remains a significant hurdle in healthcare. The lack of standardized data exchange and the presence of proprietary systems hinder the seamless flow of information, impacting care coordination and patient outcomes.
Continue Reading

Electronic health records (EHRs) have revolutionized the healthcare industry, streamlining patient care, improving efficiency, and enhancing communication among healthcare providers. Here, we explore the history of EHRs, highlighting the obstacles overcome throughout their development and implementation, as well as the challenges that persist for this transformative technology.
The Emergence of Electronic Health Records
The concept of electronic health records began to emerge in the 1960s with early attempts to digitize medical records. However, it wasn’t until much later in the century that technological advancements paved the way for the modern EHR systems. Standardization of medical terminologies and coding systems played, and continue to play, a crucial role in enabling data exchange and interoperability.
Overcoming Obstacles
Technical challenges
One of the initial obstacles in developing EHRs was the lack of interoperability among various systems. Different healthcare organizations and providers used numerous technologies and formats from various vendors, making it difficult to share and exchange patient information. In some cases, this is still the case.
Efforts have been made to standardize medical terminologies and coding systems, such as the International Classification of Diseases (ICD-10) and the Systematized Nomenclature of Medicine (SNOMED), to facilitate and streamline data exchange. For those new to medical coding, there are many “ICD 10 coding explained” resources available online. These resources are invaluable in understanding how these systems work. However, additional efforts are still required to achieve full interoperability.
Privacy and security concerns
The digital nature of EHRs raised concerns about patient privacy and data security. Protecting sensitive health information and ensuring data integrity became critical challenges. Legislation, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, was introduced to address these concerns and impose strict privacy and security regulations.
Robust encryption methods, access controls, and audit trails were implemented to safeguard patient data, among other protocols.
Continue Reading
 The Triple Aim framework has emerged as a guiding principle for healthcare organizations seeking to optimize patient care outcomes while simultaneously containing costs.
The Triple Aim framework has emerged as a guiding principle for healthcare organizations seeking to optimize patient care outcomes while simultaneously containing costs. In the previous articles, we discussed the importance of healthcare interoperability and the factors hindering its progress. In this final part, we will explore potential solutions and future directions to accelerate the advancement of interoperability in healthcare.
In the previous articles, we discussed the importance of healthcare interoperability and the factors hindering its progress. In this final part, we will explore potential solutions and future directions to accelerate the advancement of interoperability in healthcare.

