May 8
2013
The Reasons for and Benefits of an ACO
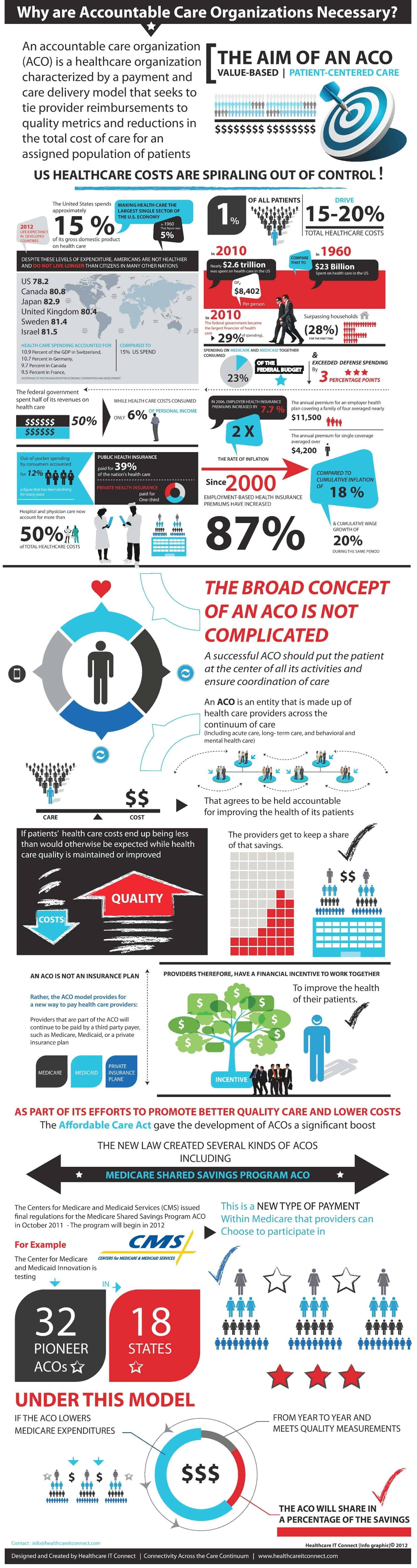
Wondering why ACO’s are necessary has become somewhat of a routine task, but there’s really very little question about the validity of the concept in that is does put the patient first. As we know, the goal of an ACO is to achieve cost and quality improvements, and a better approach to coordinated care on all levels.
There’s no doubt the majority of the responsibility for a successful implementation of an ACO lies with physicians. If adopted as a model, physicians are forced to lead us forward; however, the details depicted in the image below (thanks to Healthcare IT Connect for compiling it) tell a much broader and deeper story that clearly paints a picture of troubling times ahead unless something is done about this trend.
Having spent a portion of my career on both the payer and HIT sides, much of this information comes as no surprise, but it’s still troubling nonetheless that health plan premiums have risen 87 percent since 2000 while American’s wage growth is only up 20 percent in the same period, as depicted below for example.
Especially incredible, though, is that hospital costs amount for 50 percent of all the healthcare costs in this country. Staggering.
One of the reasons the ACO model is so intimidating is that one cannot control the reimbursement. In most cases, payment received is for services rendered. Nothing new here. But putting a portion of one’s payment “at risk” is risky for the provider. I deal with this type of payment model on occasion. For clients that want to incentive my performance, they hold a portion of my hourly fee back until certain goals are met. Once I’ve been held accountable, I receive my predetermined inventive.
I’d rather have the guaranteed funds up front, but at least I know that the quality of my work depends on my performance and better performance leads to more money in my pocket. In the end, my own personal ACO model works for all parties involved, and if it doesn’t (on rare occasions), no one comes out ahead.