Dec 10
2019
Creating A New Community Integrated Health System: Role of the Traditional Health Provider
By Leslie Wainwright, PhD., chief funding and innovation officer, Parkland Center for Clinical Innovation (PCCI).
Addressing the social determinants of health (SDoH) in communities is a hot topic of conversation in healthcare. The industry has bought into the theory that 20 percent of an individual’s health is determined by clinical care and the rest by social, economic, genetic and behavioral factors. But perhaps more importantly health systems need to recognize that they can’t solve this issue on their own.
From my perspective at PCCI, I’ve seen an increase in value-based contracting models in recent years, and health systems and physicians are looking beyond the four walls of their institutions to build relationships with outpatient, behavioral health, post-acute care, and now non-medical providers. The number and types of collaboratives between health systems and non-traditional providers has been growing over the past several years with a recent report gathering information on more than 200 different partnerships between hospital and community-based organizations across the country.
But while health systems may be embracing community provider relationships, I believe that sustainable success in addressing social determinants of health requires a fundamental shift in the way health systems view their role in improving the health of their communities.
Over the past ten to fifteen years there has been an evolution in how health systems have approached improving health outcomes. Initially health systems focused on providing high-tech solutions for care delivery such as robotic surgery, and advanced imaging techniques. Then to meet the need for increased access and demand for outpatient services, health systems seeded service areas with ambulatory surgery centers, urgent care, retail clinics, and physician offices.
In each of these evolutions the strategies centered on a solution created by the health system alone. And one could argue that the main beneficiaries of these investments were often the health systems themselves – increased market share, improved reimbursements. But such a self-centered approach will not work when addressing social determinants where the root causes lie outside the four walls of the health system.
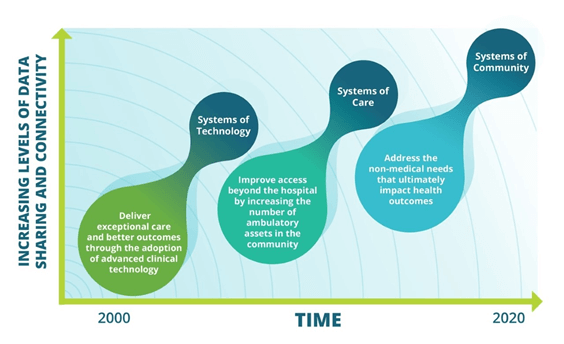
Effectively creating a system of community will require a collaborative mentality from health systems. While they may have power and influence to gather partners to the table, execution of successful interventions lies with social services and community-based organizations that are the experts in understanding and helping individuals address social needs. Even if not leading, health systems should still be active participants in this work. Indeed, there are areas where their contributions to the organization of partners is critical:
- Community Health Needs Assessment
CHNAs, which all health systems are required to complete, can be a starting point for developing strategies to address social determinants of health by quantitatively and qualitatively identifying the needs of the local community. To supplement the CHNA, additional SDoH data should be incorporated to help identify needs at the block level which can help pinpoint exactly where an intervention will likely make the most impact. These enhanced data should map and evaluate SDoH needs at the block, not zip code level, and should be supplemented with qualitative surveys to understand capacity for self-care, isolation, and learned helplessness across individuals and community.
- Governance Structure
At the core of any collaborative with community partners should be a formal governance structure that defines the policies and documentation that will enable partners to execute and measure success of their strategic interventions. A formal governance structure can also ensure that all partners have a voice at the table and may help to mitigate any fears that community organizations have that the health system is in control of the initiative.
- Legal Structure and Data Sharing
Now more than ever, technology, and indeed cloud technology, can connect disparate partners across multiple settings to exchange, share and report on data about the same community members. But there are significant legal and compliance requirements involved in sharing data across entities. Health systems have the expertise to ensure that policies around data sharing are in accordance with Medicare and HIPAA regulations. Health system experts in data privacy and security can provide advice and support to community-based providers in developing policies and procedures required to share data securely.
Improving patient engagement is at the top of the list of priorities for most health systems. The only way that a health system can achieve this is by creating strategies that start and end with the needs of the community. To find success in addressing social determinants of health, health systems will need to cede control and the notion that they need to create, lead and execute the strategy alone.
Spotlight on patient care: Dallas Connected Communities of Care
The Connected Communities of Care (CCC) platform was first implemented in Dallas in 2014 and serves as a comprehensive foundation for partnership by leveraging a web-based information exchange/case management software platform providing seamless connection and coordination between healthcare providers and a wide array of community-based social service organizations.
Since its inception, more than one million services have been documented and more than 215,000 unique individuals who have been impacted by a network of six health care systems and over 100 community-based organizations. The novel approach to addressing SDoH and organizing cross sector information sharing through sophisticated connections has garnered national recognition and has made a lasting impact in Dallas.
Not only has this collaboration connected existing organizations in a new system of community health, it has also changed the way health systems define competitors vs. collaborators. Local health systems that may have viewed each other as competitors for services, have recognized that prioritizing the needs of the community through collaboration makes a stronger impact than any isolated intervention.