Oct 27
2020
Beating COVID-19 By Shifting From Reactive To Pro-Active Care
By Dr. Donald Voltz and Eric Tran, master of science in microbiology and immunology, School of Medicine, Tulane University, New Orleans, LA.
The COVID-19 virus is ravaging the planet at a scale not seen since the infamous Spanish Flu of the early 1900s, inflicting immense devastation as the U.S. loses more than 200,000 lives and counting.
According to CDC statistics, 94% of patient mortalities associated with COVID-19 were simultaneously suffering from preexisting conditions, leaving a mere 6% of victims with COVID-19 as their sole cause of death. However, while immediate prospects for a mass vaccine might not be until 2021, there is some hope.
The fact that four in ten U.S. adults have two or more chronic conditions indicates that our most vulnerable members of the population are also the ones at the greatest risk of succumbing to the pandemic.
Healthcare providers must pay close attention to patients harboring one of 13 chronic conditions believed to play major roles in COVID-19 mortality, particularly chronic kidney disease, hypertension, diabetes, and COPD.
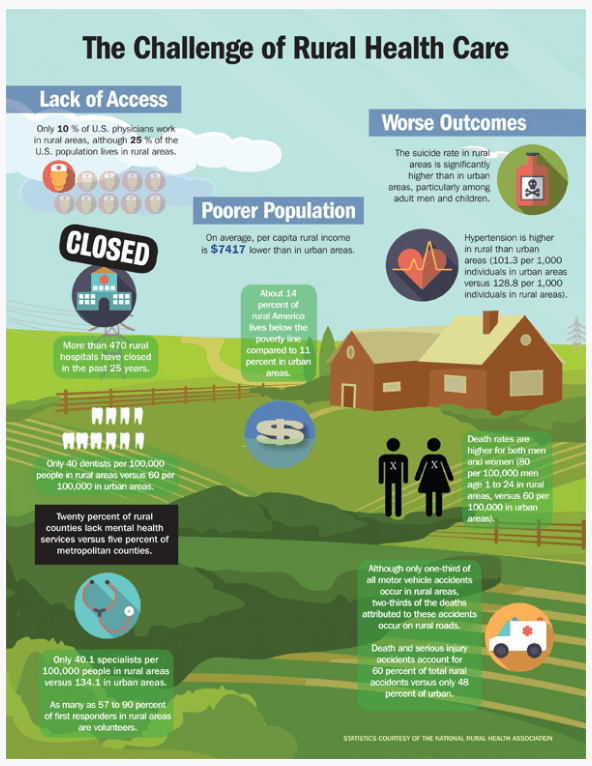
Rural populations are some of the most vulnerable and must be supervised due to their unique challenges. The CDC indicates 80% of older adults in remote regions have at least one chronic disease with 77% having at least two chronic diseases, significantly increasing COVID-19 mortality rates compared to their urban counterparts.
Health behaviors also play a role in rural patients who have decreased access to healthy food and physical activity while simultaneously suffering high incidences of smoking. These lifestyle choices compound with one another, leading to increased obesity, hypertension, and many other chronic illnesses. Overall, rural patients that fall ill to COVID-19 are more likely to suffer worsened prognosis compared to urban hubs, a problem only bolstered by their inability to properly access healthcare.