Apr 26
2019
Clinical Communication Comes of Age: Using A Mobile Maturity Model To Develop A Sustainable Mobile Strategy
By Adam Mahmud, healthcare lead, Jamf, and Si Lou, CEO, PatientSafe Solutions.
Today’s healthcare workforce is increasingly mobile. The industry has seen a dramatic increase in the use of mobile devices by both staff and patients, but often as single point solutions that do not solve for the fragmentation of clinical workflow at the point of care. Health system IT and clinical leadership are responding with a more strategic approach to clinical communication and collaboration to improve the care delivery experience at scale.
PatientSafe Solutions partnered with HIMSS Analytics to survey more than 300 healthcare leaders about the current state and future plans for mobile communication in their organizations. The vast majority of hospitals (77 percent) have invested in some form of mobile app to support communication amongst the care team, the most commonplace being secured messaging. However, clinical workflow suffers from the continued use of multiple, single-point device and applications. The average care team member — from physicians to nurses to allied health professionals – must use as many as five different devices or modalities to communicate and execute a defined plan of care.
The study also found that that nearly 50 percent of respondents plan on standardizing and consolidating onto a smartphone platform to streamline care collaboration. We all know by now that smartphones present the opportunity to deliver care at the bedside in a more effective, personalized and productive manner. However, despite investment in secured messaging and the desire to move towards smartphone-based platforms, the care team’s communication, care collaboration and documentation workflow still can be disorganized, incomplete and at worse, not secure.
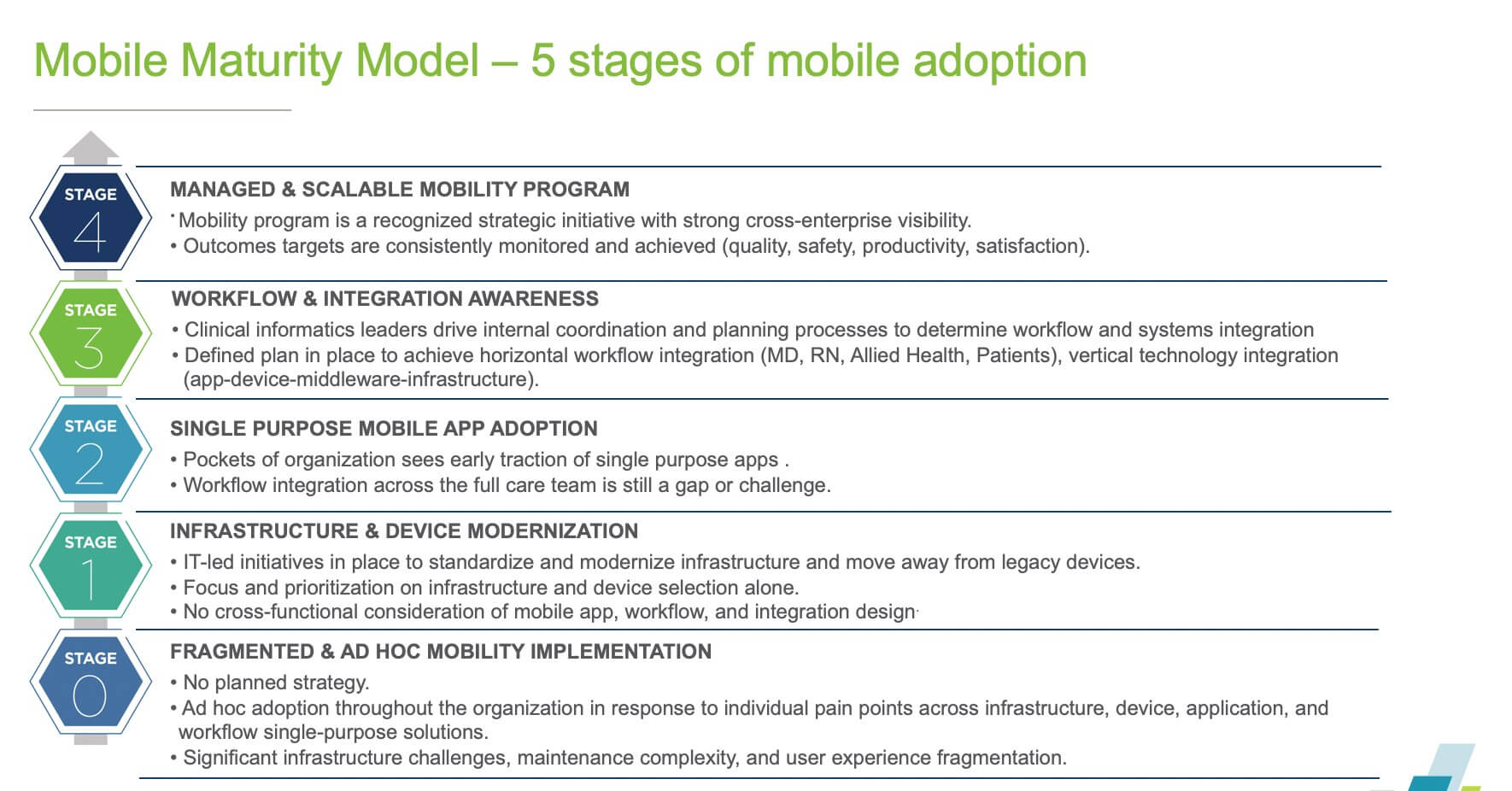 To address the clinical mobility challenge, PatientSafe developed the Mobile Maturity Model for Healthcare as common framework to assess the current state of mobile adoption in your health system and align the various people, technologies and processes to be successful with mobility at scale. Our goal? To get industry-wide participation in using and evolving the healthcare mobile maturity model – so clinicians and patients benefit from a streamlined, secure, context-rich mobile care experience.
To address the clinical mobility challenge, PatientSafe developed the Mobile Maturity Model for Healthcare as common framework to assess the current state of mobile adoption in your health system and align the various people, technologies and processes to be successful with mobility at scale. Our goal? To get industry-wide participation in using and evolving the healthcare mobile maturity model – so clinicians and patients benefit from a streamlined, secure, context-rich mobile care experience.
The Mobile Maturity Model seeks to assess and categorize an organization’s proficiency in six key capabilities: infrastructure management, mobile device management, integration planning, application selection, workflow design and outcomes management.
- Infrastructure management – To support mobility at scale, it is important to avoid underestimating infrastructure investments. Elements to consider when it comes to infrastructure include an organization’s wireless network, telephone systems and data center.
- Mobile device management (MDM) – The choice of mobile device is a key consideration in mobile adoption, but equally important is the consideration of how to successfully manage and support an entire fleet of mobile devices. Jamf, the standard in Apple device management, recently surveyed 600 global healthcare IT professionals and found that 78 percent of healthcare organizations have an MDM in place, but over 50 percent lack satisfaction, 70 percent had concerns around security and compliance, and 90 percent think their MDM can be doing more. It’s important to invest in an MDM that aligns with overall mobility strategy and are experts in the device platform selected for an organization. An MDM should have an integrated partner ecosystem for devices, applications and infrastructure and training, services and support. Indicators like customer retention and CSAT are also helpful. Most importantly, the MDM should be nearly invisible to end users, as if an approach to deployment and management hinders usability of the device an organization wants to use to improve its patient care and clinical communications, it’s not the right fit.
- Application selection – The sheer volume and variety of mobile applications available can be overwhelming. It’s important to remember that applications don’t exist in a vacuum. Infrastructure, integrations and workflow design should drive mobile app selection. An organization’s mobile maturity includes the degree to which consideration of end user experience influences application selection. As mobility initiatives continue to increase, the organizations that include clinical, informatics and IT stakeholders from mobility strategy development to implementation and ongoing outcomes management to be the most successful.
- Integration planning – Integration planning encompasses the tools, mechanisms, protocols, and standards through which structured data from source systems are processed and routed to applications on mobile device of choice. It is one of the most challenging aspects of mobile adoption as it directly impacts on the end user’s workflow. In order to optimize user experience and reduce support complexity, planning should encompass all source systems and vertical integration between network, MDM and mobile apps.
- Workflow design – Workflow design considers each user on a care team and includes the communication, documentation, coordination and executional tasks that need to be completed. In order to maximize adoption, organizations should provide for the broadest span of workflows across all roles on a care team. Technology has the potential to empower care teams to be more effective and efficient and improve care coordination and collaboration. Workflow design optimization is required to ensure that the selected technologies – applications, devices, middleware, MDM can truly enable more efficient, safer workflows.
- Outcomes management –A sustainable mobility strategy starts with the financial, operational and clinical outcomes the organization wants to achieve. Continuous monitoring and ongoing optimization is the cornerstone for a mature approach to mobility. A well-defined set of outcomes helps align design and implementation decisions down into workflow, integrations, applications, devices, MDM and infrastructure.
How can we assess where we are today?
Today, most health systems are in stage one and two, where there is a general desire to modernize infrastructure and move towards smartphones, but they have not yet pursued the true enterprise-wide, cross-functional, outcomes-led approach found in organizations in stage four. There is a need for a fundamental paradigm shift to an outcomes-driven mobility strategy, with a focus on a user-first design driven by workflow and integration planning out of the gate, to chart a path to tangible results across care quality, productivity and satisfaction.